Search the Community
Showing results for tags 'nursing home'.
The search index is currently processing. Current results may not be complete.
-
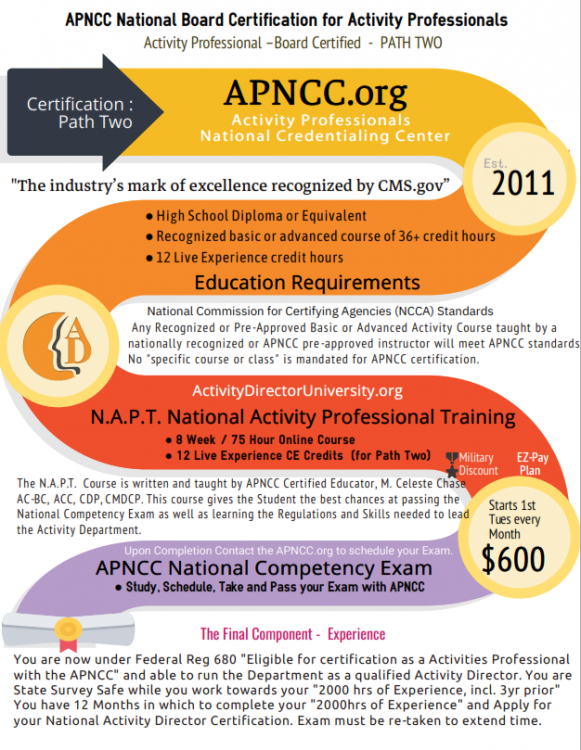
The History of Almshouses to Nursing Homes The first almshouse in United States history was founded in Boston, Massachusetts, in 1622. The original Boston Almshouse was burned down in 1682 and was rebuilt away from the heart of Boston nearly a decade later. Upon entering the almshouses in Connecticut, patients were whipped ten times. There were similar institutions developed from 1725–1773 in Pennsylvania, Rhode Island, Virginia, and New York. At the Pennsylvania Hospital, some "lunatics" were chained to a cellar wall or wore primitive straitjackets. One of the biggest problems with almshouses is that they were rarely self-sustaining. They were costly to run, and the capacity of the inmates to pay for their own keep by working at the farm, or working at the almshouse itself, was greatly overestimated. There were not enough staff, facilities were not kept up, and the poor kept coming. The Evolution 1860 Before the American Civil War, local officials regulated almshouses and did not ensure the people inside them were being cared for in the proper way or given the time they needed for help. It was not until the 1860s that more progressive states such as New York began to create boards that regulated, inspected, and reported on almshouses. 1884 The statistical analysis of the Massachusetts almshouses showed four in the city of Boston and 225 almshouses throughout the state. These almshouses housed nearly 7,000 people. Of these residents, 700 were believed to have a mental illness. Half of these almshouses did not house children. Almshouses were often multiple small terraced houses or apartments providing accommodation for small numbers of residents. The units may be constructed in a "U" shape around a communal courtyard. Some facilities included a chapel for religious worship. 1878 The Newark almshouse opened in September 1878 as a branch of the Syracuse State School. It was located on 104 acres of land within the town of Newark, New Jersey, and held around 853 patients. The nine dormitory buildings that housed the patients were able to hold anywhere from 45 to 130 people. There was also a small hospital within the almshouse that could hold up to 30 patients. There were not many employees, only about 110, to take care of the hundreds of young women admitted to the almshouse. Patients were committed to the Newark State School by superintendents of the poor as well as judges who declared them insane or feeble-minded in court. By the end of the 1800s, almshouses began to be replaced by asylums and institutions. Before the nineteenth century, no age-restricted institutions existed for long-term care. Rather, elderly individuals who needed shelter because of incapacity, impoverishment, or family isolation often ended their days in an almshouse. Placed alongside the insane, the inebriated, or the homeless, they were simply categorized as part of the community's most needy recipients. Centuries in the Making 19th Century In the beginning of the nineteenth century, women's and church groups began to establish special homes for the elderly persons. Often concerned that worthy individuals of their own ethnic or religious background might end their days alongside the most despised society, they established—as the founder of Boston's Home for Aged Women (1850). Throughout the 19th century almshouses were a last resort for those who were poor, disabled, and elderly. Residents experienced mistreatment, destitution, and inhumanity. Almshouses continued into the 19th century, until activists sought to remove children, the mentally ill, and the developmentally disabled from all almshouses and increase the number of institutions, hospitals, and asylums for them to reside in. In 1910 the state of Massachusetts, reported that 2,598 persons resided in such asylums. The great majority of these individuals were widowed and single women who had lived their entire lives, or at least a great proportion, as citizens of the state. Despite the name changes and the rosy descriptions that filled the institutions' annual reports, most people hardly looked upon the almshouse as a satisfactory solution to the demands for long-term care for the elderly. By the 1950s, the intent of policymakers to destroy the hated almshouse had clearly succeeded. Most poorhouses had disappeared from the landscape, unable to survive once their inmates no longer received federal annuities. As a result, and due to the lobbying of public hospital associations, Congress amended Social Security to allow federal support to individuals in public facilities. According to investigations of the industry in the 1970s, many of these institutions provided substandard care. Lacking the required medical care, food, and attendants, they were labeled "warehouses" for the old and "junkyards" for the dying by numerous critics. 21st Century In the twenty-first century, nursing homes became a standard form of care for the most aged and incapacitated persons. Nearly 6 percent of older adults are sheltered in residential facilities that provide a wide range of care. While these aging individuals no longer face the horrors of the almshouse, the development of the modern-day industry reflects its historical roots. In establishing monthly annuities for the old and disqualifying all residents of public institutions, the creators of Social Security took direct aim at the despised poorhouse. In shutting the almshouse door, policymakers gave birth to the modern nursing-home industry. https://en.wikipedia.org/wiki/Almshouse https://www.4fate.org/history.pdf Have a topic request or question for Celeste? Send them over to celestechase@activitydirector.org Next NAPT Class for Activity Director Training December 7th Activity Directors Network was founded in 1996 on the idea that we could help create elderly care that dramatically improved the lives of those we all serve. We envision facilities that feel like homes and that celebrate our resident’s individuality and allows them to live with dignity, purpose and joy. We believe the exchange of education and wisdom between the most talented teachers and passionate students is the way to make an impact. Each and every single one of you are the revolution that is changing everything. Thanks for being a part of The Network. Copyright © 2021 Activity Directors Network, LLC All rights reserved. Our mailing address is: 2810 US HWY 190 W Ste 100-A9 Livingston, Texas 77351
-
- apncc
- activity director certification
-
(and 2 more)
Tagged with:
-
View this email in your browser The Unsung Hero of Long Term Care Facilities The COVID-19 pandemic has come in like a lion (through infection); ruthlessly and relentlessly devouring the physical well being of the individual from which this disease takes claim. The other less recognized, less publicized, and profoundly less understood yet equally sinister devastation bestowed by this infection is the retaliatory affects of social isolation and other psychological stresses affecting our aging population living in nursing homes during this pandemic. In addition, the sudden onset of COVID-19 has unceremoniously and expeditiously eliminated the once familiar daily routines that residents have come to know and expect. The Challenges The impact of current pandemic related stressors and social isolation cannot be overstated. Facilities have justifiably but abruptly ended group stimulation, social interactions and temporarily paused self-directed choices that have been deemed necessary to reduce high risk infection spread for facility residents and the staff. Long Term Care Facilities’ residents suddenly and unexpectedly find themselves confined to their rooms without social dining, interest based group pursuits, and no longer allowed to have in-person family visits. Emotional disruptions of such magnitude may perpetuate mental health conditions such as, post-traumatic stress (PTSD), depression, loneliness and anxiety that may lead to life-threatening status and failure to thrive. Highly elevated emotional stressors may be detrimental to the functioning of the individuals’ immune system. Additionally, elevated loneliness, anxiety, and unrelenting fears may further lead to a number of deleterious consequences, such as high blood pressure, depression, and suicidal thoughts. The Unsung Heroes Claim Their Place Amongst the tenacious and dedicated nurses, doctors, and therapists is a member of the Interdisciplinary Team that goes unnoticed. These healthcare professionals work day in and day out in the midst of this pandemic to support the emotional health of our elderly population living in Long Term Care facilities. These are the Long Term Care nursing home “Unsung Heroes” of the Covid-19 epidemic. The nursing home Therapeutic Programming Professional takes responsibility for resident “engagement” and partners closely with the other IDT members in the continuum of care dedicated to delivering “whole health and wellness”. These professionals create facility programming intended to support the residents’ emotional well being which in turn, greatly helps to reduces imposed epidemic related stressors. Consequently, leading to better immunity and that is a “golden ticket” with unlimited value. These professionals focus on the residents’ personal interests and individualized needs. They create the pathway for each unique resident so they may continue enjoying the same leisure quality of life interests which they had previously come to treasure during their lifetime. Supporting the residents’ choice to continue enjoying deep roots preferences allows them to continue being connected to their personal identity well into aging years. The Spirit to Succeed One can only imagine the immense challenges brought on by the pandemic social distancing and mask infection control practices or the spirit and tenacity these professionals must draw upon to support and maintain resident connectivity at a time when imposed limitations curtail even the best of those well laid out plans. These programs may help residents spend time constructively, thereby decreasing loneliness and anxiety while maintaining social distancing. In addition, these trained professionals collaborate with the clinical staff and therapists to utilize clinical & psychology approved therapeutic approaches. Here are several suggestions to help reduce social isolation and improve engagement with residents: Non-group or solitary interventions, such as laughter therapy, horticultural therapy, and reminiscence therapy, can be more effective in reducing residents’ feelings of loneliness. Staff have transformed into surrogate family members with frequent and more lengthy contacts. Have them wear photos and name tags on top of their PPE. Regular video chats with family members facilitated by social work and/or therapeutic programming staff is essential. Regular telehealth visits should be provided by doctors and other therapists. Celebratory, fun, and interesting snacks, treats, and programming (e.g., music therapy) can be brought to the door, room, and bedside. Drive-thru family visits to the facility can be set up, using masks and social distancing. Offer in rooms stimulation via video and/or closed-circuit TV. We must remember that ALL front line caregivers are true heroes, facing daily stress that can be overwhelming for the benefit of those they serve. Heartfelt gratitude to every healthcare “Essential Personnel”! Whether in Long Term Care or Hospital Critical Care, it cannot be overstated that family members and close friends lack adequate words, in any language, that will sufficiently convey the level of gratefulness and thankfulness to those devoted nurses, doctors and therapist and Therapeutic Programming Professionals that remain dedicated despite potential exposure and personal risks. From each and everyone one of us! https://www.psychiatrictimes.com/view/the-impact-of-covid-19-on-mental-health-in-long-term-care-settings Have a topic request or question for Celeste? Send them over to celestechase@activitydirector.org Buy Now We Proudly Support : Activity Directors Network was founded in 1996 on the idea that we could help create elderly care that dramatically improved the lives of those we all serve. We envision facilities that feel like homes and that celebrate our resident’s individuality and allows them to live with dignity, purpose and joy. We believe the exchange of education and wisdom between the most talented teachers and passionate students is the way to make an impact. Each and every single one of you are the revolution that is changing everything. Thanks for being a part of The Network. Copyright © 2021 Activity Directors Network, LLC All rights reserved. Our mailing address is: 2010 US HWY 190 W Ste 120 Livingston, Texas 77351
-
- activity director
- nursing home
-
(and 2 more)
Tagged with: